
Telemedicine has become a normal part of healthcare. Many organizations expanded virtual care to make it easier for patients to get care and to keep services running smoothly.
But while telemedicine grew quickly, data management often struggled to keep up.
Today, healthcare leaders are dealing with increasing amounts of virtual care data spread across multiple systems.
Clinicians switch between platforms, compliance requirements keep changing, and patients expect the same level of trust and consistency they receive during in-person visits.
This is no longer just a technology problem. When telemedicine data is not managed well, it slows teams down, increases compliance risk, and affects the quality of care.
This article provides a practical guide for healthcare leaders to manage telemedicine data effectively without disrupting care delivery, focusing on three essential pillars:
- Privacy – maintaining patient trust and regulatory compliance
- Security – supporting operational resilience and risk reduction
- Clinical continuity – ensuring consistent, high-quality care across virtual and in-person settings
- The Reality of Telemedicine Data in Healthcare Operations
- Privacy in Telemedicine: Maintaining Patient Trust at Scale
- Security Risks That Can Disrupt Virtual Care Delivery
- Building Secure Telemedicine Systems Without Slowing Operations
- Clinical Continuity: The Operational Blind Spot in Telemedicine
- Enabling Continuity Through Integrated Telemedicine Data Systems
- What the Future Holds for Telemedicine Data Management
- Conclusion
The Reality of Telemedicine Data in Healthcare Operations
Telemedicine data extends far beyond the virtual visit itself. Every digital interaction generates information that must be captured, managed, and shared across clinical and operational teams.
What Data Is Generated Across Virtual Care Workflows
Across a typical telemedicine workflow, healthcare organizations manage several categories of data.
Patient onboarding information includes demographics, intake forms, and consent or authorization records that support compliance and care readiness.
Virtual visit data captures clinical notes and assessments, diagnoses, treatment decisions, and, when applicable, audio or video consultation files generated during care delivery.
Remote patient monitoring data includes vital signs from wearables or connected devices, along with ongoing health metrics and alerts that extend visibility beyond the visit itself.
Post-visit and care coordination data consists of secure patient messages, follow-up instructions, care plans, referrals, and coordination notes that guide next steps in care.
Administrative and financial data, including billing documentation and reimbursement or coding-related information, support the operational side of telemedicine.
Each of these data types plays a role in delivering coordinated, compliant, and patient-centered virtual care.
Why Telemedicine Data Becomes Operationally Complex
From an operational standpoint, telemedicine data is rarely centralized. It is often spread across multiple platforms and systems and managed by different vendors at various points in the care journey.
As a result, clinical staff frequently transfer or duplicate information manually, and leadership teams find it difficult to view telemedicine data in a single, unified way.
As telemedicine programs scale, many organizations turn to custom telemedicine app development to consolidate data across platforms and simplify workflows.
Privacy in Telemedicine: Maintaining Patient Trust at Scale
Privacy is foundational to patient trust, but maintaining it becomes more complex as telemedicine scales.
Unlike in-person care, virtual care introduces new environments, tools, and partners into the care experience, each of which has privacy implications that healthcare leaders must actively manage.
Why Privacy Is Harder in Virtual Care Models
In telemedicine, care is delivered beyond the controlled setting of a clinic or hospital, which introduces challenges that affect both patient experience and organizational risk.
Patients often join visits from homes, workplaces, or shared spaces, increasing the possibility of unintended exposure.
Virtual care also relies heavily on personal devices such as smartphones, tablets, and home computers, which may not meet enterprise-level security standards.
Privacy concerns are further shaped by patient questions around recordings and data reuse, including whether visits are recorded, how long information is stored, and who can access it.
In addition, third-party vendors such as telehealth platforms, messaging tools, and remote monitoring providers frequently handle sensitive patient information outside core clinical systems.
For healthcare leaders, these factors make privacy a visible part of the patient experience rather than solely a backend compliance issue.
Regulatory Expectations Healthcare Leaders Must Account For
While regulations vary by region, most healthcare organizations must address privacy expectations across several areas.
These responsibilities include the protection of electronic protected health information under HIPAA in telehealth, as well as managing consent for virtual visits, recordings, and digital communication.
Organizations must also support patients’ rights to access, correct, and understand how their data is used, along with cross-border or remote care considerations when patients or providers operate in different jurisdictions.
Operational Privacy Best Practices That Actually Work
Effective privacy management must fit real clinical and operational workflows.
This includes designing telemedicine processes with privacy built in from the start, implementing role-based access aligned with clinical responsibilities, and ensuring consent is clearly captured and documented within virtual care systems.
Organizations also need to maintain audit trails that leadership teams can easily review and define vendor accountability through clear contracts and policies.
When privacy is embedded into daily operations, patient trust is protected without slowing care delivery.
Security Risks That Can Disrupt Virtual Care Delivery
As telemedicine becomes a core service line, security incidents increasingly disrupt direct care.
For healthcare leaders, security is not just an IT concern, it is also an operational and clinical risk.
Common Telemedicine Security Threats
Many security challenges in virtual care stem from scale and complexity rather than advanced attacks.
Common risks include ransomware incidents that disrupt scheduling systems or virtual clinics and insecure video platforms deployed without proper configuration.
Weak authentication practices during peak clinical hours further increase risk when speed takes priority over security.
Additional exposure comes from API vulnerabilities between telehealth platforms, EHRs, and third-party tools, as well as phishing attacks that target staff working remotely.
These threats typically exploit gaps between systems, processes, and human behavior rather than technical weaknesses alone.
The Real Cost of Security Failures for Providers
The impact of a security incident extends well beyond data loss. Healthcare organizations may face cancelled clinics and delayed patient care, along with loss of patient trust and increased churn.
Operational downtime and recovery costs often follow, accompanied by heightened regulatory scrutiny and additional reporting obligations.
Security incidents also place significant strain on clinical and IT teams, contributing to increased stress and burnout.
In virtual care environments, even short disruptions can cascade across multiple services, making proactive security planning essential to maintaining reliable, patient-centered telemedicine programs.
Building Secure Telemedicine Systems Without Slowing Operations
For many healthcare leaders, the challenge is not whether to strengthen security, but how to do so without adding friction to already busy clinical workflows.
Effective telemedicine security must support care delivery rather than obstruct it.
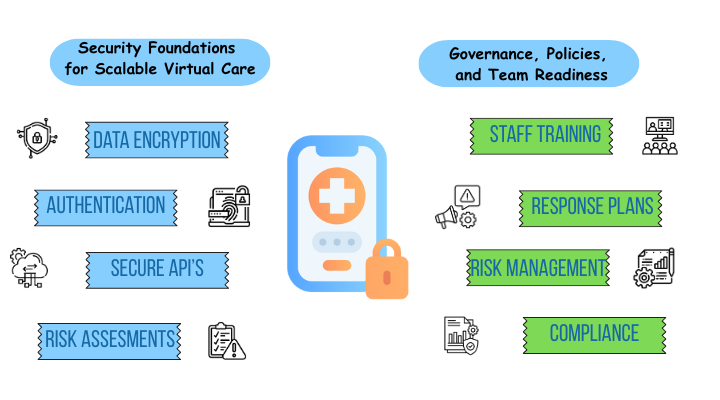
Security Foundations for Scalable Virtual Care
Scalable virtual care programs depend on core security practices that operate in the background while allowing clinicians to remain focused on patients.
Encryption protects patient information during virtual visits, data transfers, and storage, forming the foundation of telemedicine security.
Multi-factor authentication is designed to provide strong protection without slowing clinicians down, particularly during peak clinical hours.
Secure APIs support safe data exchange between telemedicine platforms, EHRs, and third-party tools, reducing risk as information moves across systems.
Regular risk assessments aligned with telehealth workflows ensure security reviews reflect how virtual care is actually delivered.
These assessments are often strengthened through telehealth consulting services that help align security controls with real-world clinical operations.
Healthcare-compliant cloud infrastructure further supports scale while meeting security and compliance requirements.
Governance, Policies, and Team Readiness
Technology alone is not enough to ensure telemedicine security.
Security is most effective when ownership and accountability are clearly defined across IT, compliance, and operations, with responsibilities shared rather than siloed.
Staff training must also reflect clinical realities. Short, role-specific training programs are more effective than generic or time-consuming approaches and are more likely to be adopted in busy care environments.
Clear incident response plans are equally important. Teams need to understand exactly what actions to take when a security issue occurs, before an incident disrupts care delivery.
As telemedicine ecosystems continue to grow, vendor risk management becomes a critical security function.
Effective oversight ensures that third-party partners handling sensitive data meet organizational security and compliance expectations.
Clinical Continuity: The Operational Blind Spot in Telemedicine
While privacy and security receive significant attention, clinical continuity is often the most overlooked aspect of telemedicine data management.
Yet continuity has a direct impact on care quality, clinician efficiency, and patient outcomes.
What Clinical Continuity Means in Hybrid Care Models
In hybrid care environments, clinical continuity depends on data moving seamlessly across care settings.
For providers, this means creating smooth patient journeys between virtual and in-person visits, maintaining complete visibility into patient history across care settings, and enabling consistent clinical decision-making across teams and departments.
Well-integrated telemedicine data allows clinicians to focus on delivering care rather than searching for information.
How Poor Data Management Breaks Continuity
Fragmented telemedicine data quickly breaks clinical continuity.
Providers commonly experience: Missing clinical context during virtual visits, duplicate tests or repeated patient questions, conflicting records across systems, and increased cognitive load on clinicians who must piece information together manually.
Over time, these issues slow care delivery, frustrate staff, and undermine patient confidence.
Addressing clinical continuity requires treating telemedicine data as a shared clinical asset—not isolated information tied to a single platform.
Enabling Continuity Through Integrated Telemedicine Data Systems
As telemedicine programs scale, healthcare organizations reach a critical inflection point.
Point solutions and disconnected platforms may work during early adoption, but over time, they create fragmentation that undermines privacy, security, and clinical continuity.
At this stage, interoperability becomes essential, serving as a technical enhancement and as a strategic decision about how virtual care fits into the broader care delivery model.
Without integrated data flows, organizations rely on manual processes and duplicated documentation to bridge gaps between systems.
These workarounds increase compliance risk, expand the security surface area, and disrupt clinician workflows.
Over time, they erode trust in telemedicine and limit the ability to scale virtual care safely and efficiently.
Interoperability as a Leadership Decision
Many organizations treat interoperability as an IT responsibility, even though it directly affects clinical and operational performance.
When driven at the leadership level, integration enables organizations to align virtual care with enterprise-wide standards for governance, security, and patient experience.
Key interoperability priorities include:
- Seamless EHR integration with telemedicine platforms
- Use of standards such as FHIR and HL7 to support consistent data exchange
- Real-time synchronization of clinical information, including visit notes, medications, referrals, and care plans
Enabling Continuity and Outcomes Through Integration
Organizations that integrate telemedicine data create longitudinal patient records, reduce duplication, and enable more consistent clinical decision-making across virtual and in-person care.
Integration transforms telemedicine data from isolated encounter information into a shared clinical asset that improves care coordination and outcomes.
What the Future Holds for Telemedicine Data Management
As virtual care matures, telemedicine data management is evolving with broader healthcare technology trends.
AI-powered documentation helps reduce administrative burden, while zero-trust security ensures continuous verification across users and systems.
Patients gain more control over their data, and telehealth regulations provide clearer guidance on privacy and security.
At the same time, organizations are consolidating point solutions into unified platforms, creating more integrated digital care ecosystems.
These trends point to a future where telemedicine data management is more automated, secure, and closely aligned with clinical and operational goals.
Conclusion
Telemedicine success now extends beyond the ability to conduct video visits.
As virtual care becomes a permanent part of healthcare delivery, how organizations manage telemedicine data plays a central role in determining quality, efficiency, and trust.
Privacy, security, and clinical continuity are deeply interconnected, and weaknesses in one area often create challenges across the entire care experience.
By treating telemedicine data as a strategic asset instead of a technical requirement, organizations can scale virtual care more responsibly.
Strong data foundations help healthcare leaders build trust, reduce risk, and deliver consistent, effective virtual care.






