
If you go to a hospital waiting room on a Monday morning, you will see many people waiting. The chairs are not comfortable.
The staff members keep getting asked how much longer the wait will be, making everyone feel stressed, which is strange for a place meant for healing.
Hospitals buy expensive new machinery and invest millions in medical technology while patient flow remains stuck in 1995.
This slow system actually costs hospitals more than patient care. Slow systems leave patients frustrated and confused, and convince them to write bad reviews online or spread negative word of mouth about your brand.
Some patients might even skip their next doctor’s appointment, directly impacting the revenue opportunities. This leaves hospital staff tired and stressed, and they spend more time dealing with the mess than actually helping people.
The answer to this problem is not to hire more staff or build bigger waiting rooms. The real answer is to change how patients move through the hospital.
Modern healthcare queue management systems and an efficient floor plan can help healthcare facilities solve the patient flow problem. It should not just be added later as a quick fix.
- Core Challenges in Healthcare Queue Management
- Building Healthcare Operations That Actually Work
- Map Every Patient Touchpoint
- Ask the Hard Operational Questions
- Integrate Process, People, and Technology
- Design Systems Around Real Workflows
- Key Features of an Ideal Queue Management System in Healthcare
- Implementation: Workflow + System Deployment Steps
- Key Benefits Facility & Patients Will See
- Conclusion
Core Challenges in Healthcare Queue Management
Most hospitals think their only issue is the long wait line, but the real problem is how the work gets done. The queues are just where the bad workflow shows up.
Let’s see the core challenges staff members face:
When Traditional Methods Fall Short
Manual ticketing systems do not work well when too many people show up. People with appointments mix with those who just walk in, and staff cannot easily tell who needs help first. This causes a long wait for a short visit.
Sometimes, morning appointments take so long that afternoon visits start very late. Staff lose track of who arrived first because the paper logs are messy.
Patients who were on time see others who just walked in get seen sooner. This is a problem with the system, not the people. Working harder will not fix it.
Impact on Patients and Facility Performance
Long waits do more than just make patients upset. They cause people to miss their appointments. This means doctors lose time and the hospital loses money. Patients write bad reviews online and suggest that others not visit your hospital.
The hospital staff spends time managing the lines instead of caring for the sick. The staff members have zero clue when rooms are empty or too full.
Poor patient flow makes things worse and causes staff to quit their jobs. To stop this, the hospital must plan the whole patient visit better.
Building Healthcare Operations That Actually Work
A good workflow plan is what makes some hospitals work well, and others struggle. This helps find spots where things slow down.
Finding these “bottlenecks” stops them from ruining the care. Even great technology will not help if you do not have a good plan first.
Here is what a good workflow plan needs:
Map Every Patient Touchpoint
Good workflow design looks at the full trip a patient takes. This trip includes many steps:
- Arrival (when they get there)
- Check-in
- Triage (when staff decide how urgent their case is)
- Waiting
- Service Delivery (getting help from the doctor)
- Checkout
- Follow-up
Mapping all these steps shows exactly where things slow down and why. Knowing these problem areas helps you stop delays before they happen. This is better than trying to fix them after everything is already messed up.
Ask the Hard Operational Questions
A queue management system in healthcare only works well if it is planned using truthful answers to questions like:
- “Where are patients waiting too long?”
- “Are staff too busy or not busy enough?”
- “How do walk-ins affect scheduled appointments?”
- “Are rooms full, or is communication about availability poor?”
A new system will fail if it is just forced onto processes that are already not working.
Integrate Process, People, and Technology
Modern queue solutions are more than just buying new computer software. They need several things to work together well:
- Changing how the work is done (process redesign).
- New rules for the staff (protocols).
- Clear ways to talk to patients (communication standards).
- The new computer system (technology).
All these parts must work together. If hospitals buy a new system but do not change their old ways of working, they will fail. All parts must match up to make things better for a long time.
Design Systems Around Real Workflows
Technology should help the way you already work, not tell you how to work. Most times, new queue systems fail because hospitals expect the computer program to fix everything. They want the software to fix their broken processes.
Instead, you should fix your workflow plan first. Then, you should use technology that helps those find better ways of working. This makes sure the new systems improve your daily work instead of making it harder.
Key Features of an Ideal Queue Management System in Healthcare
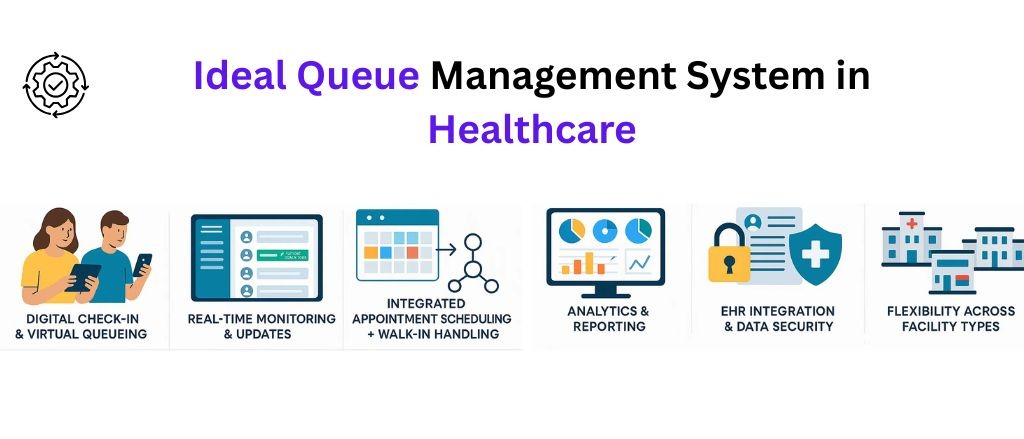
The best system does more than just handle the waiting lines. It manages the movement of patients through the whole hospital. Here’s how it helps:
Digital Check-In & Virtual Queueing
Using a queue management system, patients can check in to their queues using their phones or hospital websites instead of waiting at the front desk. This moves the bottleneck away from one spot. Walk-ins can join the line from far away and come when it is almost their turn. This cuts wait times and makes the lobby less crowded. It also helps stop the spread of sickness.
Real-Time Monitoring & Updates
Staff can see who is waiting, how long they have waited, and how urgent their needs are. Patients get texts or app alerts with wait times and updates if there are delays. This clear information makes patients less worried. They stop asking staff “how much longer?” When patients know what is happening, they handle reasonable waits much better.
Integrated Appointment Scheduling + Walk-In Handling
The system puts all patients into one single line. This includes people with appointments and people who just walk in. Scheduled patients get to go first. But, walk-ins are still tracked and helped.
Appointment scheduling in healthcare becomes dynamic; if a patient cancels an appointment last minute, the system quickly moves the next walk-in forward. This means staff do not have to manually fix the schedule. Patients do not wait longer than they should.
Analytics & Reporting
The system keeps track of the average wait times and how long each service takes. It also tracks the busiest times and how often people do not show up. These numbers help the hospital figure out where to focus its efforts.
For example, the data might show that every morning is chaotic because everyone books a 9 AM appointment. The hospital can then change the schedule to spread out those visits. Or, the data might show that some doctors always take 20% too long. This tells the hospital they need to build in more time for those appointments.
EHR Integration & Data Security
The system connects to patient electronic records. This shares info automatically, meaning fewer mistakes and less typing. Patient privacy is a must. The system also helps send high-risk patients or returning patients to the right doctors who already know their history.
Flexibility Across Facility Types
A large hospital has different needs than a small dentist’s office or diagnostic center. The new system must change to fit your hospital’s work rules. You must be able to change things like priority rules and waiting line logic. This makes sure the technology helps your daily work.
Implementation: Workflow + System Deployment Steps
Rolling out digital queue management is not quick or easy. It is not like simply plugging in a device.
Here is the plan for how to do it without causing chaos:
Assess Facility Needs
You must start by looking at your data. Ask these questions:
- How many patients do you see?
- How many people walk in versus how many have appointments?
- When do the long waiting lines start?
- Where are the current processes going wrong?
Talk to the staff at the front desk, the nurses, the doctors, and the patients. They will tell you exactly what the problems are. You just have to ask them and really listen to what they say.
Engage Stakeholders Early
Everyone who works at the hospital goes through the patient flow. This includes doctors, office staff, IT workers, building managers, and people at the front desk. You must include all of them when you pick the new system and change the workflow.
When the staff helps design the new way of working, they will want it to succeed. If you do not include them, they might fight against the changes. That resistance will make the whole project fail.
Select the Right System
Choose the system based on what you actually need, not just a list of features. Ask yourself: Do you need the system to connect with your EHR? Mobile check-in? Multi-location support?
Make sure the vendor understands healthcare (not all queue systems do), and verify they handle compliance requirements. Test the interface with actual staff who’ll use it daily, if they find it clunky, it won’t get adopted.
Pilot Testing & Staff Training
Start the new system in only one department first. Or, start it when the hospital is not busy. Collect feedback from staff and patients. Find where the new process is causing problems. Then, fix the workflow before you use the system everywhere.
You must train the staff well. Teach them the new ways of working and how to talk to patients. Understand that people will need time to learn. Plan to have extra support available during those first few weeks.
Track, Analyze, Iterate
Putting the system into place is not the end. Use the analytics to find new problems that are slowing things down. Keep making the priority rules better.
Change the staff schedules as needed. What works well in the first month might need changing by the third month. This can happen as the number of patients changes. Or, it can happen when staff find smarter ways to use the new system.
Key Benefits Facility & Patients Will See
When workflow design and technology align properly, the changes are noticeable within weeks.
Reduced Wait Times & Improved Satisfaction
Patients spend less time waiting and more time getting help from the doctor. They get clear information about any waits. This makes them less worried, even when there are delays.
More patients will keep coming back to the hospital because people prefer going to places that value their time.
Fewer Overcrowded Waiting Rooms
When patients can join the line remotely on their phones, fewer people crowd the waiting rooms. This makes the area safer and more organized. This creates a better space for the few people who need to wait there.
Higher Staff Efficiency
Staff do not need to spend as much time on problem handling and more time on patient assistance. An automated check-in system minimizes the efforts of the front desk staff.
Staff can see the waiting line in real-time. This means nurses and doctors know who is next without having to ask all the time. This saved time goes toward better talks with patients and better medical work.
Better Resource Utilization
Rooms stay filled, providers maintain a steady flow, and idle time drops. Staff scheduling aligns with actual demand rather than guesses. You’re not paying people to sit idle during slow periods or scrambling to cover unexpected surges, predictive analytics smooth out those peaks and valleys.
Transparency & Communication for Patients
Getting updates right away and being able to wait remotely reduces being unsure. Being unsure is often more frustrating than the actual waiting.
Patients feel like they know what is happening and that they are respected. This changes how they feel about the whole visit.
Conclusion
Queue problems in hospitals are not small issues. They are big system failures. These failures make patients unhappy and leave hospital staff tired and stressed. They also cause the hospital to lose money.
But here is the good news: The issue of patient flow could be resolved with a clever workflow plan, innovative queue solutions, and forecasting analytics. Start small. Start pilot. Analyze the results in one department first before you use them in the whole hospital. Most successful plans follow a pattern: test, learn, adjust, and then grow.
Those hospitals that fail are the ones that attempt to make changes all at the same time. They fail to involve the staff and make early mistakes. The goal is not just shorter waits. It is about creating smoother patient visits, reducing staff stress, and using resources better. Most of all, it is about building a reputation for respecting the patient’s time.
The technology exists. The workflows are proven. The question is whether you’re ready to move past “that’s how we’ve always done it” and build something better. Because your patients and staff both deserve operations that work as hard as they do.

 By
By 

