
Bringing artificial intelligence (AI) into your healthcare organization sounds exciting until you start asking what it’s actually going to cost. And no, it’s not just a software license.
There’s data to clean up, systems to integrate, staff to train, and infrastructure to upgrade. Along with a list of compliance boxes to check before you even get to “go live.”
Some clinics manage to get early pilots off the ground for under $300K. But for large-scale, enterprise-level rollouts, it’s not unusual to see budgets hit seven figures.
Still, there’s a strong case for moving forward: analysts project that AI could help the U.S. healthcare system save $150 billion per year by 2026, roughly $460 per person.
So the question is: What are you really paying for? And how do you know if it’s worth it?
Next, we’ll break down the cost of implementing AI in healthcare: what’s included, what usually gets overlooked, and how to make smarter investment decisions from day one.
Let’s dive in.
- TL;DR
- What Does “AI Implementation” Mean in a Healthcare Context?
- The True Cost Components of Implementing AI in Healthcare
- How Implementation Choices Impact Total Cost
- Ongoing and Long-Term Costs Many Organizations Underestimate
- Cost Ranges by Healthcare AI Use Case
- Cost vs Value: How Healthcare Leaders Should Think About AI ROI
- How to Control and Optimize the Cost of AI in Healthcare
- Bottom Line: AI Is an Investment, Make Sure It Pays Off
- FAQs
TL;DR
No time to read the full article right now? Here’s what you need to know:
- AI in healthcare comes with hidden costs: data, integration, compliance, and ongoing maintenance are often bigger than the software itself.
- Choosing between off-the-shelf tools and custom-built solutions can shift your budget by hundreds of thousands. So, plan for what you actually need.
- A small pilot can help you avoid overbuilding too soon and catch adoption issues early before they turn into rework.
- Many long-term costs get missed during planning, like model retraining, audits, and staff readiness. So, budget for the full lifecycle.
- ROI isn’t just about cost savings. Implemented correctly, AI can improve workflows, reduce burnout, and strengthen patient outcomes system-wide.
- Want to stay in control? Start small, roll out in phases, and build with people (not just tech) in mind.
What Does “AI Implementation” Mean in a Healthcare Context?
Adding AI to your healthcare system might sound simple on the surface until you try to make it work in real life.
Because in healthcare, AI changes how your systems connect, how your team works, and how you handle decisions tied to real patients, real outcomes, and real regulations.
Let’s say you’re rolling out an AI model to predict readmissions. To make it usable (and safe), you’ll need:
- Structured clinical data from your EHR and other sources; clean, consistent, and accessible in real time.
- Well-defined workflows that tell your team exactly how to act on AI-generated insights.
- Staff who are trained and confident using the tool during actual care delivery.
- Compliance across the board, including HIPAA, GDPR, and any local or national regulations.
And here’s the challenge: most healthcare systems weren’t designed with AI in mind. So making it fit often means aligning legacy tools, getting multiple teams on the same page, and tightening every step where small errors could create bigger risks.
Common AI Use Cases in Healthcare
Most clinics and health systems exploring AI fall into one (or more) of these categories:
- Virtual assistants and chatbots: Handling basic triage, appointment booking, or FAQs so staff can focus on higher-value tasks.
- Predictive analytics: Flagging patients at risk of complications, missed follow-ups, or readmission.
- Medical imaging analysis: Helping radiologists and specialists process scans faster and more accurately.
- Clinical decision support: Recommending treatment paths based on past data, medical guidelines, or patient history.
- Billing and RCM automation: Speeding up revenue cycles, spotting coding errors, and reducing denials.
- Remote monitoring AI: Tracking chronic patients and triggering alerts when something’s off.
Each use case comes with its own price tag and a different level of complexity behind the scenes.
Video to add:How AI can heal healthcare | Edmund Jackson | TEDxNashville
The True Cost Components of Implementing AI in Healthcare
There’s no flat fee for AI in healthcare, but the main cost buckets tend to show up again and again. And most clinics underestimate how many areas are involved.
Here’s where your money usually goes:
- AI software and licensing costs. This includes any tools, models, or platforms you license, subscribe to, or build. Costs vary based on scope, features, and how much customization is needed.
- Data acquisition, preparation, and governance. Before any AI tool can deliver value, you need quality data. That means collecting, labeling, cleaning, and organizing it. Plus, setting the right rules around how it’s accessed and maintained.
- Infrastructure, cloud, and computing resources. Some systems need more power than your current setup can handle. Cloud storage, computing power, or internal servers may need to be scaled up to support your AI tools reliably.
- Integration with EHRs and clinical systems. Your AI tool has to plug into what you already use: EHRs, lab software, imaging tools, or scheduling systems. Making those connections smooth and secure takes planning, time, and money.
- Staffing, talent, and training costs. You’ll likely need technical staff (in-house or external) to manage implementation and model oversight. On top of that, clinical teams need training to understand how to use the system in real time.
- Regulatory, legal, and compliance expenses. Everything needs to be aligned with HIPAA, GDPR, and local privacy regulations. That might include extra documentation, internal reviews, or hiring external compliance advisors.
- Cybersecurity and risk management investments. New digital tools mean new potential entry points. Your data security protocols might need upgrades to keep everything locked down and avoid breaches.
Pro Tip:Worried about how AI handles sensitive data? Before investing in infrastructure and security, check our breakdown on the main privacy concerns with AI in healthcare.
A Quick Breakdown of Operational Costs
Now let’s put some numbers on the board.
These estimates come from healthcare AI deployments that are already live, and they show just how quickly costs can add up once you move from planning to execution.
Here’s what operational spending might look like, according to Orangesoft’s breakdown:
- Data prep and management: $50K to $250K
- Integration with existing systems: $148K to $350K
- Regulatory compliance and security: $10K to $150K+
- Team expertise: $65K to $290K+
The gap between the low and high ends depends on your system’s complexity. It also comes down to how much internal support you already have, and how many parts of the workflow the AI needs to touch.
Some clinics can keep costs lean by building on top of what they already use. Meanwhile, others find out mid-project that their infrastructure or staff just aren’t ready yet. And that’s where budgets tend to spiral.
How Implementation Choices Impact Total Cost
Not every healthcare organization needs to go all in on day one. But the decisions you make early (what to build, how to launch it, who to involve) will shape your entire cost structure.
Some choices lower the barrier to entry, while others raise the stakes (and the budget) fast. The key here is understanding how each option affects time, scope, and long-term value.
Let’s break down the most common decision points that can shift your total cost in a big way:
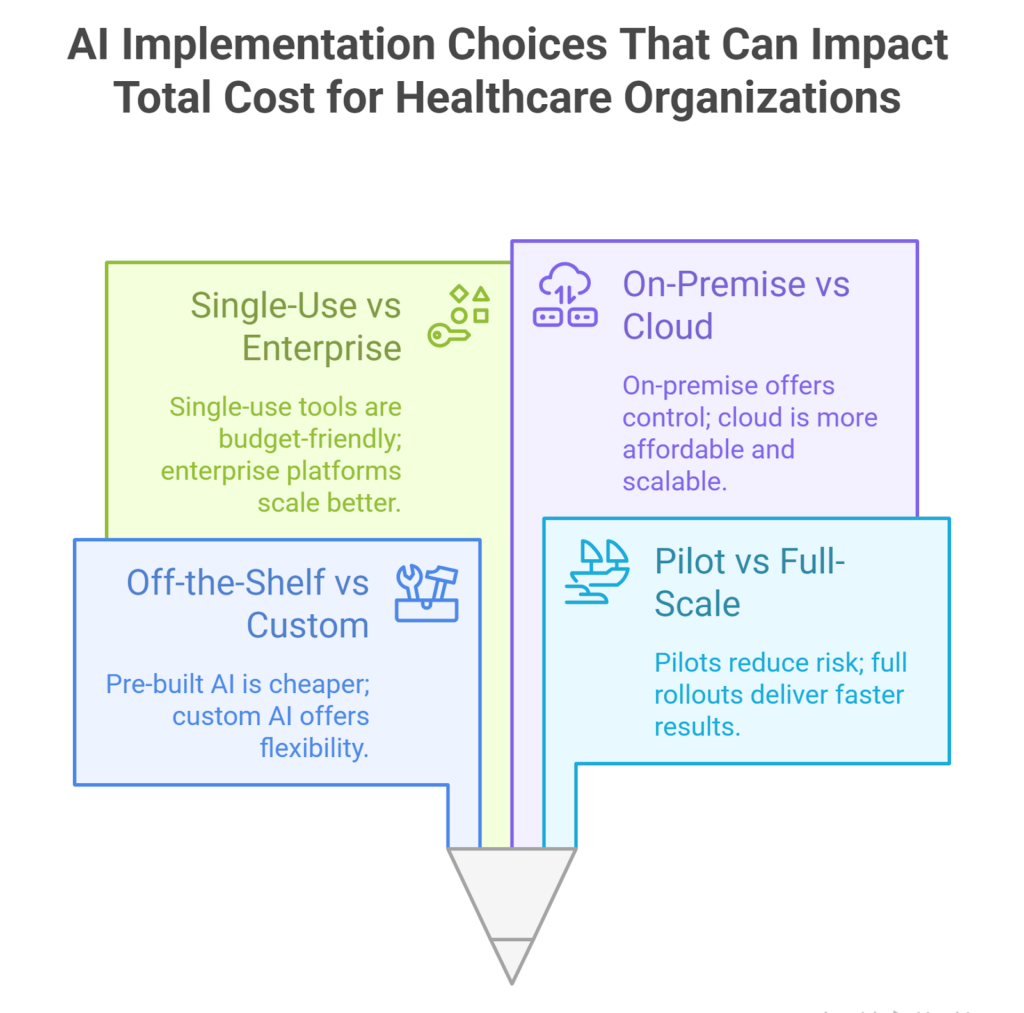
Off-the-Shelf vs Custom-Built AI Solutions
Pre-built tools are faster to deploy and easier on the budget.
According to Itrex, adding basic AI features to an existing healthcare app can cost around $40,000, especially if there’s minimal training involved.
But when you need more control (let’s say, a tool built around your workflows or clinical data), costs go up fast.
- A decision tree model for predicting patient readmission might cost $35,000–$45,000.
- A deep learning model for cancer diagnosis or treatment planning can reach $60,000–$100,000.
- Full, custom-built AI systems often land well over $100K, depending on scope.
Off-the-shelf works when your needs are simple. But for anything mission-critical or deeply integrated, custom builds give you the precision and flexibility that off-the-shelf tools can’t match.
Pilot Programs vs Full-Scale Deployment
Pilots are a smart way to keep costs down while testing functionality in a real setting. You limit risk, gather feedback, and avoid betting everything on day one.
Full deployments, on the other hand, mean more upfront investment but faster system-wide impact if things go well.
Most clinics benefit from starting small and scaling with proof. Just make sure your pilot is designed with growth in mind, or you’ll pay for avoidable rework later.
Single-Use AI Tools vs Enterprise-Wide Platforms
Some clinics start with one tool for one task, like an AI chatbot for appointment reminders or a model to flag high-risk patients. These single-use tools, often powered by conversational AI or basic predictive models, are more affordable upfront and easier to implement.
But once you start layering multiple tools, integration gets tricky.
That’s when enterprise-wide platforms become a better option. They’re built to connect across departments, manage data centrally, and scale over time.
Enterprise platforms come with higher costs, often $1M or more. But they also create long-term efficiency and better ROI if AI is part of your broader care strategy.
On-Premise vs Cloud-Based Architectures
Hosting your AI system on-premise gives you full control over data and infrastructure, but it comes with high setup and maintenance costs, plus heavier demands on internal IT.
Cloud-based solutions, meanwhile, reduce upfront costs and make it easier to scale. You also get faster access to updates and support, especially when working with external vendors.
If data residency or security requirements are strict, an on-premise system might be necessary. However, for most organizations, cloud-based AI is the more practical (and budget-friendly) starting point.
Ongoing and Long-Term Costs Many Organizations Underestimate
Budgeting for AI doesn’t stop once the system goes live. In fact, some of the most critical costs show up after implementation; quietly, over time, and often without warning.
Orangesoft’s breakdown also notes just how significant these long-term investments can be. Here’s how they typically stack up as a percentage of the total AI implementation cost:
- Infrastructure upgrades: 15% to 30%. If your tech stack wasn’t ready for AI from day one, chances are you’ll need to revisit it later. Especially as workloads grow.
- Model improvement and retraining: 25% to 45%. AI models don’t stay sharp on their own. You’ll need to retrain them as new data comes in or patient behaviour shifts. This is one of the most underestimated cost lines.
- Regulatory updates and audits: 10% to 20%. Compliance isn’t a one-and-done task. Changes to HIPAA, GDPR, or national frameworks can trigger the need for system reviews or recertification.
- Talent acquisition or training: 5% to 15%. AI tools evolve fast, so should your team. You might need to bring in new talent, train your current staff, or both. Either way, it takes consistent investment.
- Patient and user onboarding: 5% to 10%. Even the best tools fall flat if no one uses them. Expect to spend time and budget on adoption strategies, from education materials to support channels.
Now, what makes these costs tricky is that they don’t always show up right away. They tend to build over time, until you’re suddenly dealing with reduced performance or avoidable rework.
Planning for these variables upfront won’t eliminate them. But it does give you more control over how and when they hit.
Cost Ranges by Healthcare AI Use Case
Not all AI projects hit the same budget, and that’s exactly how it should be.
A chatbot for patient reminders doesn’t belong in the same pricing tier as a system that analyzes MRIs or connects across your entire network.
To have a better idea, Shadhin Lab’s 2025 data gives us a solid frame of reference based on the size of your organization and the type of AI solution:
| AI Solution Type | Small Org | Medium Org | Large Org |
| AI Chatbots | $50K–$75K | $75K–$150K | $150K–$200K |
| Predictive Analytics | $200K–$300K | $300K–$450K | $450K–$600K |
| Medical Imaging AI | $300K–$500K | $500K–$700K | $700K–$900K |
| End-to-End Integration | $1M–$2M | $2M–$3.5M | $3.5M–$5M |
These numbers cover more than just the tool itself. They reflect everything needed to make it work inside your organization, like infrastructure, integration, compliance, and ongoing support.
Are you looking for something like predictive analytics or medical imaging? Then, expect higher spend tied to the complexity of the data, the stakes of clinical decision-making, and the number of users involved.
For smaller clinics, a $50K chatbot might be a great first step. For larger systems, a $3M rollout makes more sense when you’re coordinating across locations and specialties.
The key here? Instead of the most expensive system, you need the one that fits where you are right now.
Cost vs Value: How Healthcare Leaders Should Think About AI ROI
Yes, AI can be expensive. But the bigger question is: what does that investment get you back?
Let’s look at the numbers. Per DemandSage, the average ROI for AI in healthcare is $3.20 for every $1 spent, with most returns kicking in around 14 months after implementation. That’s not a bad timeline when you’re improving operations, outcomes, and patient experience all at once.
But ROI doesn’t always mean cutting costs. Sometimes, it’s about building long-term capability:
- Automating admin frees up staff and reduces burnout.
- Predictive tools help prevent expensive hospitalizations.
- Better diagnostics reduce missteps and unnecessary follow-ups.
- AI chatbots improve patient engagement and cut no-shows.
- Smart triage means patients get the right care faster.
Bottom line: AI delivers value on multiple levels. But only when it’s aligned with clear goals, supported by the right team, and implemented with the long game in mind.
How to Control and Optimize the Cost of AI in Healthcare
AI doesn’t have to drain your budget, but it needs a strategy. The difference between a project that scales and one that stalls is usually in the early planning.
Here are four smart ways to keep costs in check:
- Start with high-impact, low-complexity use cases. Don’t aim for an enterprise rollout on day one. Begin with a tool that solves a clear problem and is easy to integrate, like patient follow-up automation or appointment triage.
- Use phased rollouts to stay in control. A limited launch lets you test, adjust, and prove value before scaling. It also helps you identify gaps in training, infrastructure, or adoption, without paying for all of it upfront.
- Evaluate vendors carefully and build flexible contracts. Get clear on what’s included, what support looks like, and how pricing will scale. Choose partners who understand healthcare realities, not just generic AI providers.
- Invest in internal readiness. Even the best AI system fails without buy-in. That means training your team, assigning ownership, and building workflows around the tool.
The clinics that get this right treat AI like a long-term capability, not as a quick fix.
Bottom Line: AI Is an Investment, Make Sure It Pays Off
As you could see, AI budgets can vary widely. Some clinics spend $40K, while others invest $4 million. It all depends on what you’re building, how prepared you are, and where you want the system to take you.
What’s clear is this: the cost of implementing AI in healthcare implies data, training, infrastructure, compliance, and long-term upkeep. But it also opens the door to improvements in efficiency, outcomes, and patient experience.
If you’re thinking about AI, don’t just ask how much it costs. Instead, ask what it’s worth for your clinic, your staff, and your patients over the next five years.
And if you’re not sure where to start, Medical Flow is here to help, from first consult to full implementation, and everything in between.
Talk to our team and let’s find out what AI could look like in your organization.
FAQs
How much does it cost to integrate AI technologies into healthcare practices?
It really depends on what you’re trying to build. Some clinics roll out a basic AI tool for under $100K in initial costs. Others invest millions for a full system that runs across departments.
The key is knowing what kind of impact you’re aiming for, and what your current setup can actually support.
What are the main cost components of implementing AI in healthcare?
You’re not just paying for a tool. The real costs usually come from data preparation, EHR integration, staff training, compliance, and sometimes tech upgrades. These are the pieces that make artificial intelligence in healthcare function as part of your daily operations.
What factors most influence the total cost of AI adoption in healthcare?
A few things have the biggest impact: the complexity of the AI, how many systems it needs to connect with, how specific the solution has to be, and how prepared your internal team is. For many healthcare organizations, coordination between teams is what drives the cost up the most.
How do AI implementation costs differ between hospitals and smaller clinics?
Smaller clinics can usually get started with less, especially using cloud-based tools and vendor-managed services. Larger healthcare providers often aim bigger from the start, which drives costs up, but also brings more system-wide impact.
What challenges make AI budgeting and cost estimation difficult in healthcare?
The toughest part are the costs you don’t see coming. Things like model retraining, regulation updates, or low staff adoption tend to show up months after launch. That’s why your budget should be flexible enough to adapt as you continue to use AI in more areas of your workflow.
What long-term financial and operational benefits can AI deliver in healthcare?
You’ll likely see faster workflows, fewer manual errors, better patient follow-up, and stronger team efficiency. Many clinics report a positive ROI within 12 to 18 months, especially when they start with focused use cases.






